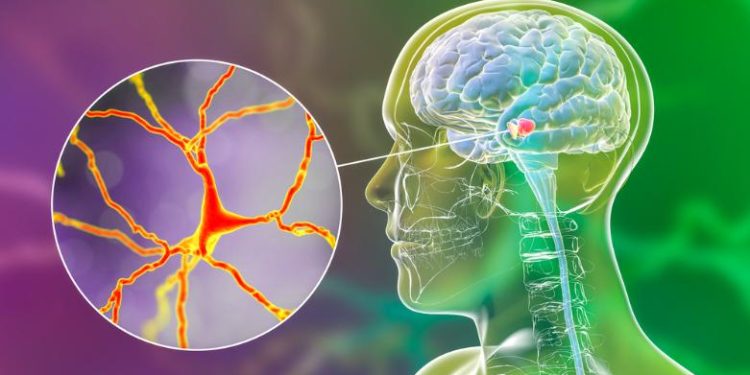
MS attacks axons in the central nervous system, which carry visual, muscle and other signals. This damages the myelin sheaths that protect them and slows or stops nerve signals from reaching the brain.
The symptoms vary, and the disease can be hard to diagnose. Your doctor will use tests like spinal fluid analysis and evoked potentials. Treatment focuses on speeding recovery from attacks, reducing new relapses and slowing disease progression.
Symptoms
The exact cause of MS isn’t known, but it is thought that something triggers the immune system to attack the central nervous system. It’s also unclear why some people develop it while others don’t, although there are some patterns. For example, it tends to occur more often in women than men. And it’s more common in families with a history of the disease.
Symptoms vary from person to person, depending on which part of the central nervous system is affected and how severely. They can include weakness, numbness or pain in your arms or legs, trouble walking or vision problems, and memory and thinking problems. Fatigue is another very common symptom, and it can be physical (tiredness in your arms or legs) or cognitive (slowed processing speed or mental exhaustion).
Some symptoms happen only during a flare-up, called a relapse, while others may persist or get worse over time. In the past, it was difficult to diagnose MS because symptoms can be similar to those of many other diseases and can change from one day to the next. But today, a thorough medical history and certain tests can help your doctor determine whether you have MS. These tests may include an MRI scan, which uses large magnets and sound waves to make detailed pictures of organs and structures inside your body. Your doctor may also order a sample of the liquid that cushions your brain and spinal cord, called cerebrospinal fluid, to check for inflammatory cells and other signs of MS. Your doctor may also perform evoked potential tests, which use electrodes placed on your skin to measure the electrical response of your nerves to different stimulation.
Treatments for MS focus on slowing the progression of disease, reducing attacks and their severity, and managing symptoms. Your doctor may prescribe steroids to reduce inflammation, muscle relaxants or antidepressants for spasticity, and medication such as clonazepam or gabapentin to control tremors. He or she may suggest exercise programs, dietary changes and stress reduction therapies to manage fatigue. Some doctors also offer individual psychotherapy, group therapy or support groups for family members of people with MS.
Diagnosis
MS affects the central nervous system, which consists of the brain, spinal cord and optic nerves. It’s an autoimmune disease, which means that your immune system mistakenly attacks healthy tissue in the central nervous system. This disrupts the transmission of nerve signals and causes symptoms. Symptoms of MS can vary widely from person to person and can come and go over time.
Some people develop very mild symptoms. Others become severely disabled. The first symptoms of MS usually occur between the ages of 20 and 40. Women are more than twice as likely to get the disorder as men. Genetics may play a role, but scientists think that an environmental trigger is also needed for MS to develop. Smoking, exposure to household chemicals and a certain infection (the Epstein-Barr virus, which causes mononucleosis) all increase the risk of developing MS.
Symptoms can affect any part of the body. They can be as mild as pins and needles, or as severe as a loss of control over your bladder. The most common symptom is weakness in the legs and arms. People with MS can also have problems with memory, speech and vision. Some develop a feeling of shock-like or burning pain in the face, called trigeminal neuralgia. This is a chronic pain condition that can be treated with medications.
The diagnosis of multiple sclerosis depends on the type of symptoms and the pattern of changes seen on imaging tests, especially an MRI. There are several different MRI scanning techniques, and your health care provider will select the best one for you.
An MRI is a diagnostic test that uses large magnets, sound waves and a computer to make detailed pictures of organs and structures inside your body. It can find areas of damage in the brain and spinal cord, as well as plaques and scarring. It can also detect damage to the myelin sheath that wraps around nerve fibers in the central nervous system. Myelin damage slows down the transmission of messages between nerve cells, and this can cause symptoms.
Your doctor will also check for other signs of MS, such as eye problems, muscle spasms and a feeling that your body is not moving properly, called ataxia. The doctors will also ask questions about your family history and personal and work histories. The doctors can then use this information to predict whether you are likely to have relapsing-remitting MS, secondary progressive MS or primary progressive MS.
Treatment
There is no cure for multiple sclerosis (MS), but treatments can help reduce symptoms, prevent relapses and slow the progression of disability. MS is a disease of the central nervous system, which includes the brain and spinal cord. Symptoms depend on the location and severity of nerve fiber damage. They can range from numbness or weakness in the arms and legs to trouble walking and balance problems. Symptoms can come and go, or they may stay the same for a long time before getting worse.
Doctors diagnose MS by performing a physical and neurological examination, asking about symptoms and considering the person’s medical history. They also use special tests, including magnetic resonance imaging (MRI), to check for changes in the brain and spinal cord. They may also perform a lumbar puncture, or spinal tap, to obtain a sample of cerebrospinal fluid for laboratory analysis to look for proteins and inflammatory cells associated with MS. They can also order evoked potentials, which test for how quickly the nervous system responds to electrical stimulation.
Medications can slow down or stop the damage to nerves by suppressing the immune system and decreasing inflammation. The drugs most commonly used to treat relapse-remitting MS are interferons, which change the way cells in the body communicate with each other. Possible side effects of these medications include flu-like symptoms, depression and elevated liver enzymes. Doctors may also prescribe glatiramer acetate, which is similar to an interferon but has fewer side effects. It works by changing the balance of immune cells in the body, and it decreases annual relapse rates and shows benefits on brain MRI scans. Other options include alemtuzumab (Lemtrada) and a Bruton’s tyrosine kinase inhibitor.
Other medicines can ease fatigue, muscle stiffness and spasms and help manage urinary and bowel problems. There are also rehabilitation programs that can improve the ability to walk, think and work and reduce pain, numbness and weakness. Psychological counseling can help address emotional changes and depression. Vocational rehabilitation can help people whose jobs have been affected by MS make career plans and learn new job skills.
Prevention
While it is not possible to prevent MS, a healthy lifestyle can reduce a person’s risk of the disease. This includes eating a nutritious diet, exercising regularly, avoiding tobacco and excessive sun exposure, controlling weight gain, and limiting stress levels. Regular medical examinations can also help to detect MS-related health problems before they cause significant symptoms.
Although it is not entirely understood, genetic factors play a role in the development of MS. People who have a close relative with the disease are at an increased risk of developing it themselves. A variant of genes known as HLA class II and HLA class I alleles is thought to increase the risk, as these genes are associated with how your body responds to inflammatory agents.
In addition, some environmental factors may be linked to MS, including adolescent obesity, low vitamin D levels, and infection with the Epstein-Barr virus (EBV), which is responsible for infectious mononucleosis. Research suggests that this virus is the most common risk factor for MS, and it appears to influence the timing of MS onset in both males and females.
Other risk factors include age (MS usually occurs between 20 and 40 years of age), sex (women are 2 to 3 times more likely than men to have relapsing-remitting MS), and location (MS is more prevalent in areas that are further north or south of the equator). A person’s hormones may also affect their MS symptoms, with changes during pregnancy, menstruation, or menopause often making them more noticeable.
The early symptoms of MS can be hard to recognize, since they are similar to many common ailments. However, if you are experiencing difficulty walking or a change in your gait (tripping and falling more frequently), numbness or pins and needles in the arms and legs, or feelings of unsteadiness and weakness on one side of the body, make an appointment with your neurologist as soon as possible.
While it is not possible to stop the autoimmune response that causes MS, there are medications that can slow down its progression. Taking these drugs along with healthy living habits can improve a person’s quality of life and reduce the severity of their symptoms.